- Join the Innovation Journey
- Our Platforms
Breakthrough lung therapy ready for clinical trials
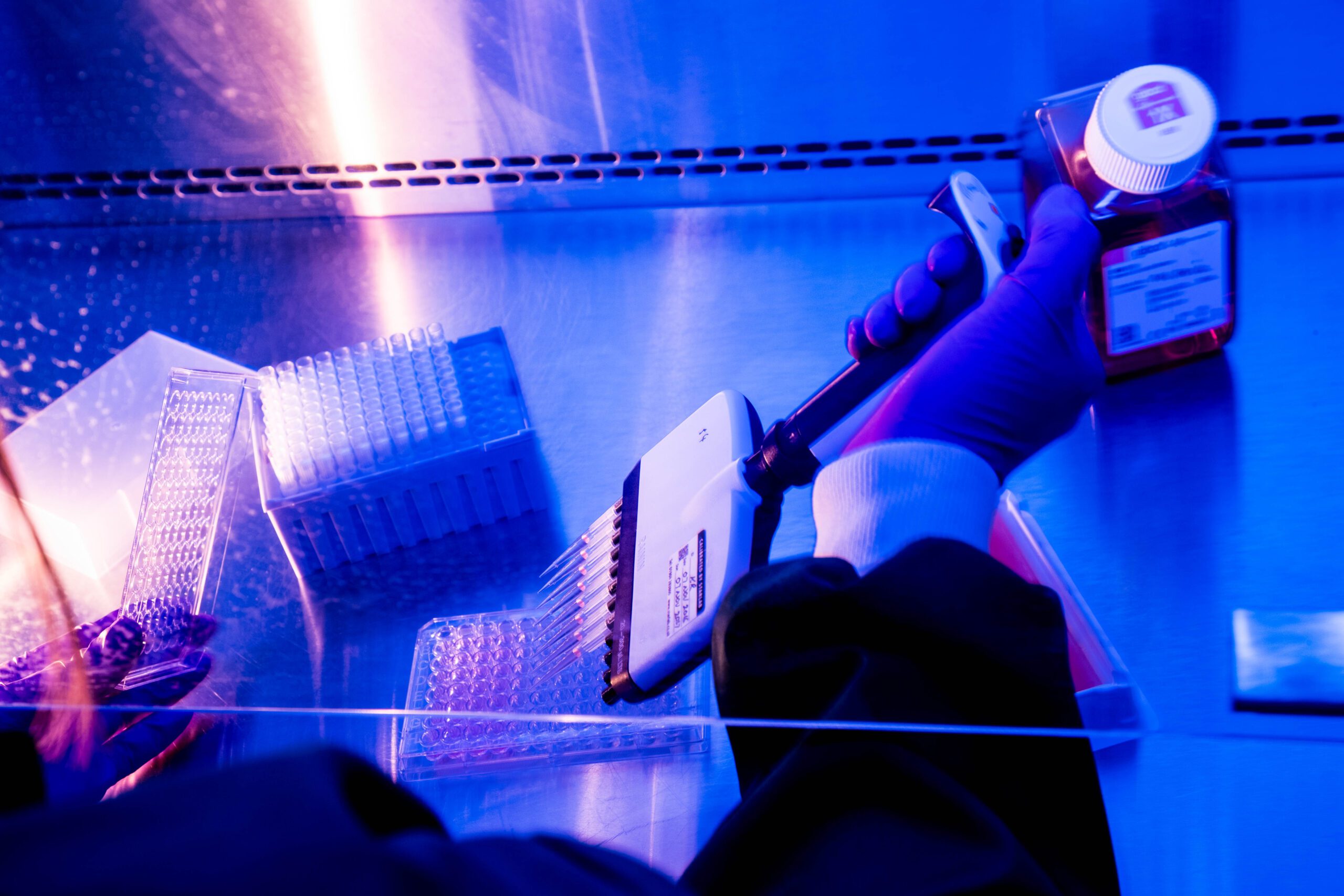
A new therapy to help the body tackle infections associated with a form of bronchiectasis, a serious and long-term lung condition, is set to enter clinical trials at The Royal Liverpool Hospital following work by the Alderley Park-based iiCON Consortium partner Infex Therapeutics.
The trial is focused on RESP-X, an anti-virulence therapy that Infex scientists have designed to help the body tackle Pseudomonas aeruginosa (pa) infections, a hard-to-treat drug-resistant pathogen recognised by the World Health Organisation as a critical threat to human health. A novel humanised monoclonal antibody, RESP-X does not kill bacteria directly but deactivates a mechanism that prevents the immune system from acting against the infection.
In particular, RESP-X tackles non-cystic fibrosis bronchiectasis (NCFB). This disease is defined by an irreversible and progressive dilatation of bronchi due to chronic bronchial inflammation. NCFB is characterized by periods of stable disease, with flare-ups, ‘exacerbations’, that increase in frequency and severity over the patient’s lifetime. In the UK the British Lung Foundation estimates there are in excess of 300,000 NCFB patients.
NCFB exacerbations are closely associated with acute bacterial infections, with Pa as one of the leading causes of infection. NCFB exacerbations are also linked with other inflammatory causes, such as viruses, inhalation of contaminants such as environmental particulates, and smoking, or other immunosuppressant factors, almost always followed by further acute bacterial infections.
Infex in-licensed the initial program from Japanese pharma company Shionogi in 2019 and its scientists have been working on RESP-X ever since, producing encouraging data in non-human trials.
The initial Phase 1a/b clinical study has been approved by the UK Medicines and Healthcare Products Regulatory Agency. It will take place at the Royal Liverpool Hospital and will be a single centre, first-in-human, double-blind, placebo-controlled, intravenous single ascending dose, to evaluate the safety, tolerability, pharmacokinetic, pharmacodynamic and immunogenicity of RESP-X in healthy subjects and NCFB patients. Patient safety, tolerability and pharmacokinetics will be assessed at each dose prior to escalation.
Having established the appropriate dose in healthy volunteers, the second part of the study will be in NCFB patients (selected to have stable NCFB and be colonised with Pa) and will look for exposure and early markers of efficacy.
Dr Peter Jackson, executive director, Infex Therapeutics, said:
“NCFB is a neglected, chronic condition that results in progressive respiratory decline and is typified by the irreversible and permanent dilation of the airways, a chronic cough, overproduction of sputum, recurrent respiratory infections and chronic inflammation resulting in progressive lung damage. Patients can become chronically infected with Pseudomonas, significantly reducing their quality of life.
“There is high, unmet need, with millions of patients worldwide at risk of this condition, and no approved preventative therapy – our RESP-X programme moving to Phase 1 is a significant step forward in creating a treatment to support patients with this unmet need.”
Professor Janet Hemingway, director of iiCON, said:
“It’s great to see RESP-X reach this milestone with iiCON support and RESP-X is typical of the exciting research the Infex team produces in seeking to bring new treatments to market that will help improve health outcomes for patients the world over.”


