- Find our latest Case Studies
- Our Platforms
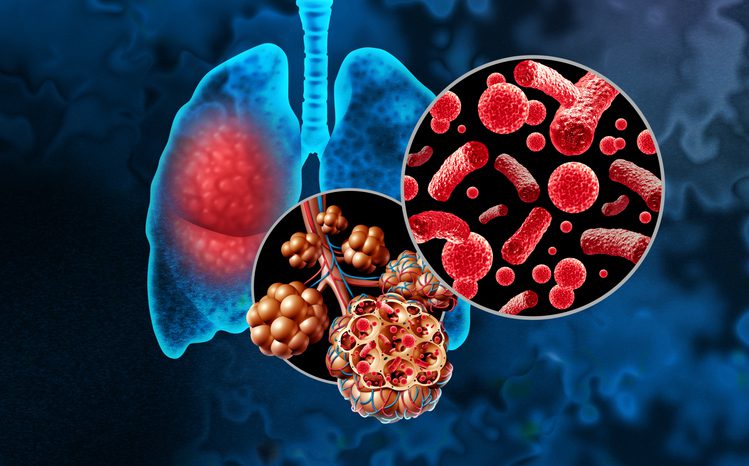
The ongoing battle to combat Tuberculosis

You may not be alone thinking that tuberculosis is a disease of the past. This infection, called consumption, phthisis or the white plague in the past, killed one in five people in the UK and Europe in the 19th Century.
Professor Luis Cuevas, Professor of International Health & Epidemiology at LSTM
Dr Peter McPherson, Reader & Wellcome Trust Fellow at LSTM
If you ask older generations, you may find relatives or family friends often died of TB. However, with improved nutrition, better housing and the development of treatment, the epidemic subsided, and most people in Europe nowadays think TB is a public health problem of the past.
Sadly, this perception is misleading. Every year millions of people become ill with TB. In 2020 alone, ten million people developed TB and 1.4 million died. TB is the second most common infectious cause of death in adults in the world – second only to COVID-19. Sadly, and almost unnoticed, more people die from TB than from other common infections such as HIV and malaria.
TB tends to be invisible and neglected: this is a disease of the poor, the malnourished, or those living with HIV. People who develop TB are often stigmatised and ashamed and have little power to make their voices heard. Even more, TB often presents with symptoms such as a prolonged cough, weight loss, and fever that are common to other conditions, making diagnosis difficult.
People with TB frequently don’t realise that they are seriously ill until the disease is advanced and are at high risk of severe illness and death, when they may have already passed the infection to others at home and their community. Many people with TB and their families experience financial ruin whilst seeking care for TB, as they often have to make many clinic visits before diagnoses, and often are unable to work for prolonged periods.
And if you think TB is not a problem in the UK…London was declared the European capital of TB, with almost 3,500 new cases in 2012. Although these numbers have decreased, in 2020, 4,125 people were notified with TB in England and, more worryingly, 11.6% of people with confirmed TB had resistance to the first-line treatment drugs. This is the highest percentage of drug resistance since the enhanced UK surveillance scheme started in 2000.
TB can be an extremely difficult to diagnose. Unfortunately, the tests available to confirm the diagnosis and whether the bacteria is susceptible to the standard treatments are far from perfect, and remain slow and expensive.
For example, the most sensitive tests, such as culture and Xpert (a rapid molecular assay) have many limitations. Culture is highly sensitive and specific, but is only available in reference laboratories and requires at least two weeks to produce results; while Xpert requires laboratory facilities with air conditioning and reliable electricity, which confines it to larger hospitals far away from the clinics.
Worse still, most people with TB attend small primary health care clinics without sophisticated laboratories, where the only test available is the 100-years old smear microscopy, which misses half of people with TB!
Not surprisingly, a major priority to improve the prevention and treatment of TB is the development of tests that are low cost, easy to use outside the laboratory and capable of providing timely results while the patient is still attending the clinic, to avoid multiple visits. The World Health Organization convened groups of experts to agree on the target product profiles (TPP) of the most needed tests (https://www.who.int/publications/i/item/WHO-HTM-TB-2014.18), but they are a tall order!
The preferred tests should screen samples other than sputum, such as urine or saliva, which requires a good understanding of the bacteria and harnessing sophisticated technologies to detect bacteria or biomarkers in low concentrations. Some current prototypes aim to detect LAM (a component to the bacteria’s wall) in urine, others screen for biomarkers in blood to develop a ‘signature’, while others aim to simplify the platforms for rapid molecular assays. However, despite many efforts, current prototypes are not there yet, as they have low sensitivity or specificity or are not suitable for the primary health care clinics.
LSTM has a long-standing interest in promoting the development of point of need tests for TB. Our work includes working with industry from conceptualisation to test development. We have a deep understanding of the conditions where the tests would be used and long term partners.
We believe there is no silver bullet solution or a one-test that fits all, but that there are potentially multiple solutions by combining imperfect tests. For example, with combinations of tests of inclusion and exclusion and using both screening and confirmatory tests, we are developing nimbler novel diagnostic algorithms that suit specific population groups.
We have international partnerships across Asia, Africa and the Americas, with whom we work evaluating early and late prototypes, either singly or in parallel and conduct implementation research to generate evidence for international guidance. We often lead large scale implementation of new tests within health systems and work in collaboration with national TB control programs for the early adoption of innovative approaches for diagnosis and treatment.